Minimally invasive orthopaedic procedures are a type of surgical technique that uses small incisions and specialized instruments to repair or replace damaged bones, joints, and soft tissue. These procedures have become increasingly popular in recent years due to their many benefits, including faster recovery times, less pain, and fewer complications. However, as with any surgical procedure, there are also risks associated with minimally invasive orthopaedic procedures.
One of the main benefits of minimally invasive orthopaedic procedures is that they cause less damage to surrounding tissues. Because the incisions used in these procedures are smaller, there is less bleeding and less damage to muscles, tendons, and other soft tissues. This can lead to faster recovery times and less pain. Additionally, minimally invasive procedures can also lead to smaller scars and a more cosmetic outcomes.
Another benefit of minimally invasive orthopaedic procedures is that they can be done using specialized imaging and navigation techniques, which can make them more precise and accurate. For example, in procedures such as total joint replacement, the surgeon can use real-time imaging to ensure that the implant is properly positioned and aligned.
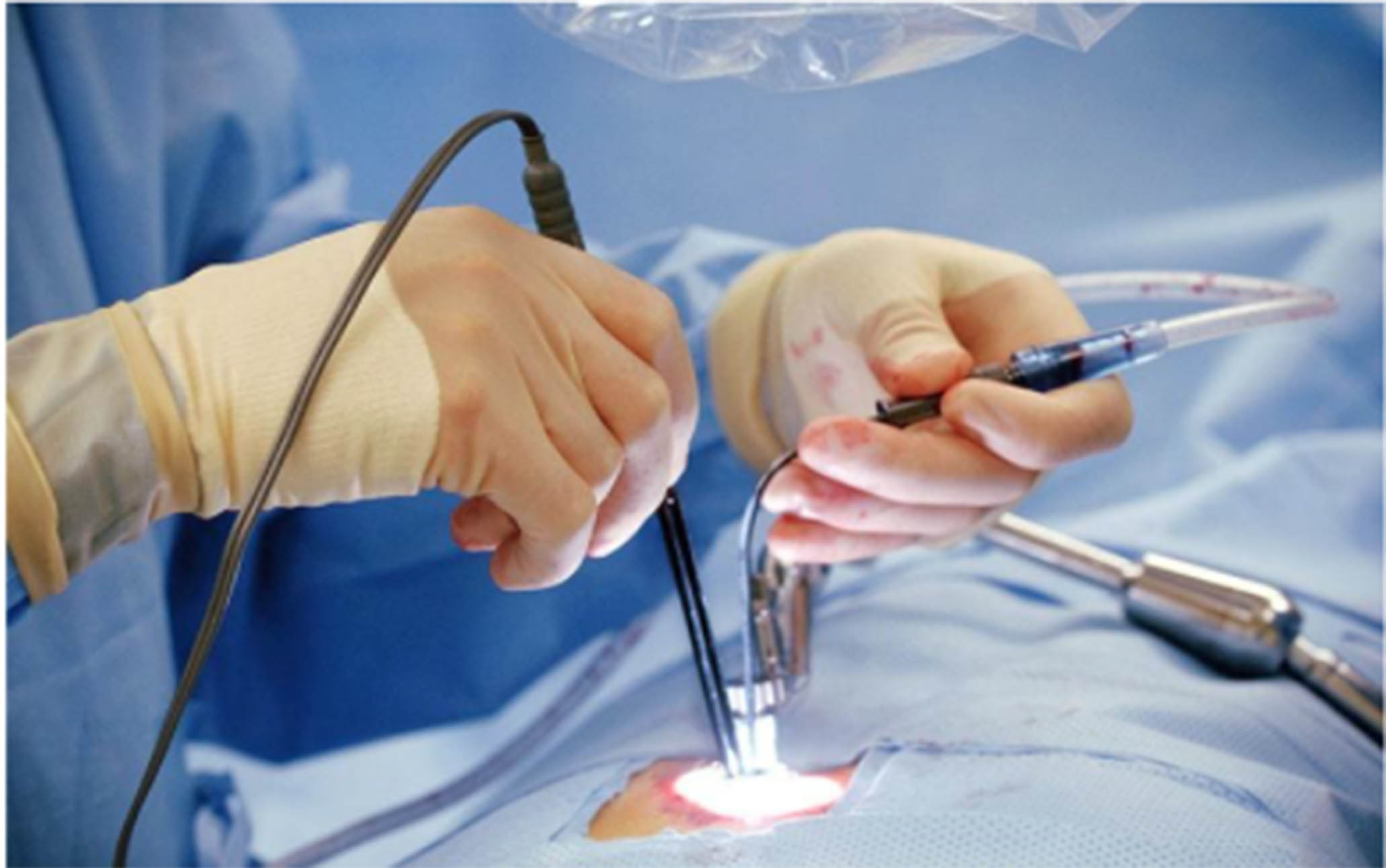
Minimally invasive procedures also have the advantage of being performed with the aid of specialized instruments, such as arthroscopy, which allows the surgeon to visualize the joint and repair the damage without making a large incision. This technique is commonly used to treat conditions such as torn cartilage, torn ligaments, or even remove loose bone or cartilage.
Despite these benefits, there are also risks associated with minimally invasive orthopaedic procedures. One of the main risks is that these procedures may not be suitable for all patients, particularly those with severe or complex injuries. Additionally, there is a risk of complications such as infection, bleeding, and nerve damage.
Another risk is that of implant failure. Implants such as artificial joints, can wear out over time, and may need to be replaced. In addition, there’s also a risk of implant infection, which can occur if bacteria enters the joint through the incision.
It’s important to note that while minimally invasive procedures are less invasive, they are still surgical procedures and carry the same risks as traditional open surgery. It’s important for patients to have realistic expectations and to discuss the benefits and risks with their orthopaedic surgeon before deciding if a minimally invasive procedure is right for them.
It’s worth mentioning that minimally invasive orthopedic procedures are not only limited to joints replacement, arthroscopy and soft tissue repairs but also includes procedures such as vertebroplasty and kyphoplasty for spine fractures, percutaneous fixation for fractures, and even certain procedures for scoliosis and spinal stenosis.
Furthermore, it’s also important to mention that not all minimally invasive procedures are the same, and some may have different levels of invasiveness. For example, arthroscopy is considered to be less invasive than an open joint surgery, but percutaneous fixation for fractures may be even less invasive than arthroscopy.
It’s also important to note that while minimally invasive procedures may have fewer complications and faster recovery times, it’s not always the best option for every patient. Factors such as the severity of the injury, the overall health of the patient, and the patient’s individual goals and preferences must be taken into consideration before deciding on the best course of treatment.
In order to make an informed decision, patients should have a thorough discussion with their orthopedic surgeon about their options, the potential benefits and risks of each procedure, and any other considerations that may be relevant to their individual case.
In conclusion, minimally invasive orthopaedic procedures are a type of surgical technique that uses small incisions and specialized instruments to repair or replace damaged bones, joints, and soft tissue. They offer several benefits such as faster recovery times, less pain, and fewer complications. However, there are also risks associated with these procedures, including implant failure, infection, and complications. It’s important for patients to weigh the benefits and risks and work closely with their orthopaedic surgeon to determine the best course of treatment for their individual needs.



